Understanding Stress, Cortisol and Pelvic Pain
By Dr. Alexsia Priolo
Research is indicating that there is a relationship between cortisol and the pelvic floor. To best understand this relationship, we must first understand stress and the body’s response to it. When the body encounters a stressor, the stressor acts as a threat to its stability. Stressors may be emotional, physical, environmental and/or chemical. Moreover, whether the stress is real, anticipated or imagined, it all has the same impact on the body.
HPA Axis
When the body recognizes a stressor, it reacts via the hypothalamic-pituitary-adrenal (HPA) axis. This is a feedback system which also regulates many body processes including digestion, immune function, mood, energy and sex.
When stress first presents itself, it’s perceived by the hypothalamus which releases corticotropin-releasing hormone (CRH), thereby acting on the pituitary gland which causes the release of adrenocorticotrophic hormone (ACTH), and finally acts on the adrenal gland which releases epinephrine (also known as adrenaline), norepinephrine and cortisol.
Epinephrine and norepinephrine are released as soon as the body perceives stress and breaks down just as quickly. Cortisol, on the other hand, is released about 10 minutes later and can circulate within the body for an hour or two after the stressor is first encountered.
Cortisol
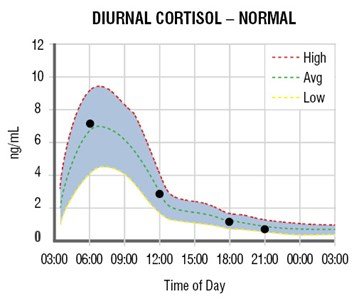
Cortisol is known as the body’s stress hormone. It follows a daily rhythm where it rises in the morning to stimulate waking and decreases throughout the day. This follows the body’s circadian rhythm which also aids in maintaining cell repair and immune restoration.
Reference: http://www.zrtlab.com/media/1476/adrenal_curve_normal.jpg?width=359&height=299
When the body experiences stress, cortisol is released by the adrenal gland; and when the body is constantly experiencing stress this may eventually lead to persistent activation of the HPA axis.
Spectrums of the Stress Response
There are two points along the spectrum of the stress response:
Alarm:
This occurs immediately once a stressor is encountered, whereby the HPA axis is activated causing a ‘fight or flight’ response. Eventually, the stressor is neutralized through the cortisol response. Symptoms on this end of the spectrum include high stress, anxiety, agitation, poor sleep, ‘wired but tired’ feeling and a high pulse.
Exhaustion:
As the body is repeatedly exposed to stressors (and cortisol), the hypothalamus and pituitary begin to lose sensitivity causing exhaustion of the HPA axis. Cortisol production is also affected as the body becomes depleted in the nutrients needed to produce cortisol.
Symptoms experienced on this end of the spectrum include: fatigue and exhaustion, tired in the evening, poor sleep and low pulse. On this end, you may also be suffering from pain, prone to allergies, unable to handle small stressors, emotional issues and slower wound healing.
Pelvic Pain and Cortisol
Several studies have confirmed a relationship between low cortisol and pelvic pain.
Endometriosis:
Cortisol awakening response was lower in women suffering from endometriosis compared to controls. Moreover, the cortisol curve was lower in the endometriosis group. This study also found that women who reported severe pain with sex had lower cortisol levels than controls. Lastly, women experiencing infertility also showed lower levels of cortisol.
Interstitial Cystitis:
Women with IC who experienced a lower morning cortisol peak, were more likely to report greater nocturnal urinary frequency (nocturia). Furthermore, those who had lower cortisol levels experienced greater pain in the lower abdomen as the bladder filled and more average nocturia and frequency of urination during the day.
Vulvovaginal Candidiasis (vaginal yeast infection):
Women with recurring yeast infections showed lower cortisol values and a blunted morning cortisol rise compared to controls. Moreover, they also showed lower average cortisol levels.
Vulvodynia:
Women with vulvodynia showed blunted morning cortisol and also experienced more symptoms of stress compared to controls.
Re-establishing a healthy rhythm
It’s clear that women who are living with pelvic pain have disruptions in their normal cortisol rhythm. One study looked at the impact of physiotherapy and psychotherapy treatments on women with chronic pelvic pain and showed that the cortisol levels were higher in women after treatment and similar to cortisol levels in healthy women.
As a Naturopathic Doctor, I believe in assessing the whole picture and looking at the root of the problem. If adrenal health is suffering because most women are in the exhaustion-end of the spectrum, we need to support the adrenals. At this point, the body is depleted in specific nutrients necessary for optimal health and function of the adrenal glands. A high quality vitamin B complex with activated forms of vitamin B is necessary for energy production and herbs like licorice are important for cortisol production.
Additionally, you can look at your own cortisol rhythm using salivary cortisol testing offered by Naturopathic Doctors. This will give an indication of how to specifically treat your cortisol pattern and allow us to use it as a baseline for treatment progression.
References:
Lutgendorf S, Kreder K, Rothrock N et al. Diurnal cortisol variations and symptoms in patients with interstitial cystitis. J Urol. 2002;167(3):1338-1343. doi:10.1016/s0022-5347(05)65295-0.
Ehrström S, Kornfeld D, Thuresson J, Rylander E. Signs of chronic stress in women with recurrent candida vulvovaginitis. Am J Obstet Gynecol. 2005;193(4):1376-1381. doi:10.1016/j.ajog.2005.03.068.
Petrelluzzi K, Garcia M, Petta C, Grassi-Kassisse D, Spadari-Bratfisch R. Salivary cortisol concentrations, stress and quality of life in women with endometriosis and chronic pelvic pain. Stress. 2008;11(5):390-397. doi:10.1080/10253890701840610.
Ehrström S, Kornfeld D, Rylander E, Bohm-Starke N. Chronic stress in women with localised provoked vulvodynia. Journal of Psychosomatic Obstetrics & Gynecology. 2009;30(1):73-79. doi:10.1080/01674820802604359.
Friggi Sebe Petrelluzzi K, Garcia M, Petta C et al. Physical therapy and psychological intervention normalize cortisol levels and improve vitality in women with endometriosis. Journal of Psychosomatic Obstetrics & Gynecology. 2012;33(4):191-198. doi:10.3109/0167482x.2012.729625.
Quiñones M, Urrutia R, Torres-Reverón A, Vincent K, Flores I. Anxiety, coping skills and hypothalamus-pituitary-adrenal (HPA) axis in patients with endometriosis. J Reprod Biol Health. 2015;3(1):2. doi:10.7243/2054-0841-3-2.
Schrepf A, O’Donnell M, Luo Y, Bradley C, Kreder K, Lutgendorf S. Inflammation and inflammatory control in interstitial cystitis/bladder pain syndrome: Associations with painful symptoms. Pain. 2014;155(9):1755-1761. doi:10.1016/j.pain.2014.05.029.
Schrepf A, O’Donnell M, Luo Y, Bradley C, Kreder K, Lutgendorf S. Inflammation and Symptom Change in Interstitial Cystitis or Bladder Pain Syndrome: A Multidisciplinary Approach to the Study of Chronic Pelvic Pain Research Network Study. Urology. 2016;90:56-61. doi:10.1016/j.urology.2015.12.040.
Lima A, Moura M, Rosa e Silva A. Prolactin and cortisol levels in women with endometriosis. Brazilian Journal of Medical and Biological Research. 2006;39(8):1121-1127. doi:10.1590/s0100-879×2006000800015.