How to Promote Success with Your Pessary
Leeanna Maher, PT, MSc PT, H.BSc
A pessary is a medical grade silicone device that sits comfortably inside the vagina. The purpose of this device is to offer an immediate resolution of symptoms that are commonly associated with pelvic organ prolapse such as pelvic or vaginal heaviness, pressure, and bulging sensation. It aims to resolve the sensation of tissues bulging and dropping down at the vaginal opening. It can even help support the resolution of urinary incontinence.
When one is fitted with a pessary, there are many strategies that can promote and ensure that the pessary will continue to provide the support needed in the long term. Let’s discuss some of these aspects in detail:
Vaginal Tissue Integrity:
For those who are in perimenopause and menopause, a decline in hormone levels decreases the production of natural vaginal secretions that lubricate the vaginal walls, plumpness, and tolerance of the vaginal tissues to the presence of a pessary. It is essential that every client is provided with guidance and direction from their primary health care practitioner on whether or not to use a local vaginal estrogen supplement or vaginal moisturizer. These products help to support vaginal tissue health and integrity, thus reducing the risk of vaginal mucosal erosions or skin breakdown. A topical estrogen works specifically to increase blood flow and promote improved extensibility of the vaginal tissues while a vaginal moisturizer rehydrates the vaginal tissues and provides moisture using hydrating ingredients.
2. Intra-abdominal Pressure Management Awareness:
Various activities throughout our day generate intraabdominal pressure (IAP) within our abdominal cavity. This occurs when the body is moving with effort or exerting such as pushing, pulling, picking up objects, sneezing, coughing, laughing, running, and even walking. The level of IAP generated varies depending on the activity. The goal is to ensure that the activation of our pelvic floor and core muscles are strong enough and timed properly to prevent the generation of excessive IAP in the downward direction. Excessive downward pressure can cause the pessary to move out of its ideal position within the vaginal canal and sometimes can even be expelled. This is especially true during bowel movements. It is very important to ensure that constipation and straining is not a complication when one is using a pessary. The straining associated with constipation often contributes to aggravating the pelvic organ prolapse and makes it more difficult for the pessary to provide the support needed. This type of training is best addressed through pelvic health physiotherapy. Pelvic health physiotherapists assess the activity of the pelvic muscles and the strategies used by the client to guide them on promoting improved strength and coordination during activities that increase IAP.
3. Routine and Consistent Pessary and Vaginal Tissue Checks:
When the pessary is initially fitted, it is important to have a committed schedule of appointments for the pelvic physiotherapist or doctor to remove the pessary and check the vaginal tissues for any signs of vaginal tissue breakdown, pressure spots, improper positioning of the pessary, and abnormal vaginal secretions (colour and/or smell). At these appointments, the pelvic physiotherapist will also ask about any concerns related to the use of the pessary such as pain, vaginal bleeding, difficulty evacuating bladder and bowels, or any slippage of the pessary. Proactive steps can be taken to address any concerns which may include removal of the pessary for a period of time to let the vaginal tissues rest/heal if required, and a new pessary can be trialed which may provide improved support. Once the pessary is inserted, the schedule of check ups may vary but generally there is a check in within the first week of use. Another follow up is generally scheduled within 4 weeks of use, followed by a 3 month, 6 month, and if all continues to be well, yearly check ups. These pessary and vaginal tissue check ups can be performed by the client’s pelvic physiotherapist or primary care practitioner and are essential to promote and increase the success of a pessary.
4. Pessary Device Inspection and Cleaning Consistency:
Pessary device inspection and cleaning consistency. If you have been fitted with a pessary that has been determined to be self managed, this means that you are able to remove and insert the pessary yourself. It is essential to remove the pessary and inspect the material at the frequency that has been communicated to you by your pelvic physiotherapist. The removal frequency can vary depending on the pessary shape and your personal needs. Inspecting the pessary means looking for any areas of the pessary that might be damaged, deteriorated, ripped or torn. If drainage holes are present in your pessary, It is important to also inspect for tears around the drainage holes. If there are rough edges, this could rub against the vaginal tissues causing tissue breakdown and irritation. It is generally recommended by Canadian pessary manufacturers to replace the pessary device once there are signs of “damage or deterioration” on the pessary. Once the pessary is removed, the recommendation is to wash the pessary thoroughly using a mild soap with water.
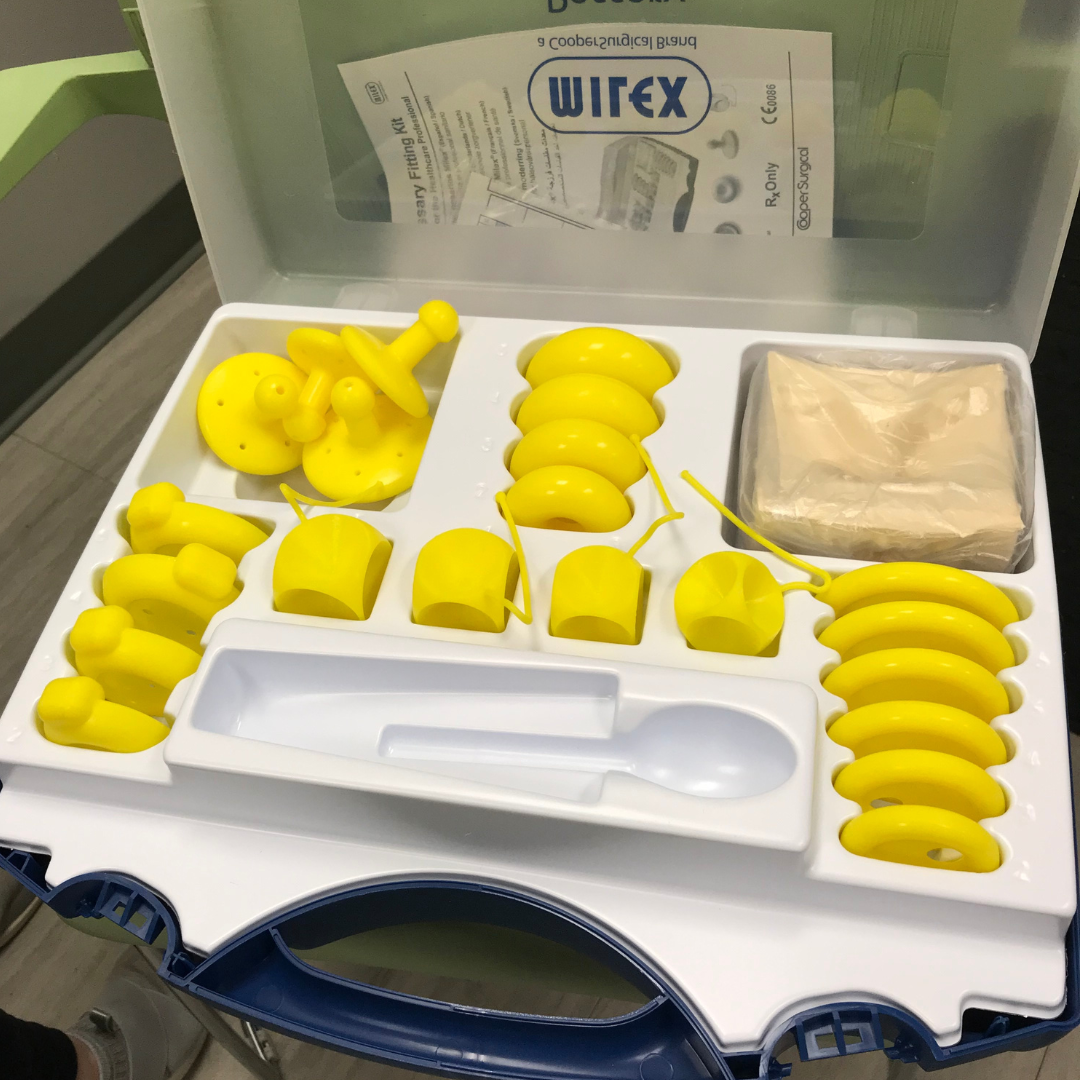
It has been reported that continued use of a pessary following an initial fitting ranges from 50-80% after 3-4 months. Taking on the responsibility of a pessary means committing to the consistent check ups initially agreed upon by the pelvic physiotherapist, gynecologist, or urogynecologist who originally sized and fit the pessary. Pessary fitting can include a period of trial and error. Although it is an optimal outcome to be successfully fitted on the first trial, it isn’t unreasonable to assume that a trial of different pessary shapes and sizes may be required to find the “perfect one”. Pessary check-in appointments are meant to troubleshoot any problems or concerns associated with the new pessary as soon as they come up. These check-ins provide continued education and support by the health care provider (pelvic physiotherapist, gynecologist/urogynecologist) to ensure that the client feels supported and more confident that they are doing everything they need to ensure the pessary’s success in the long term.
Resources: